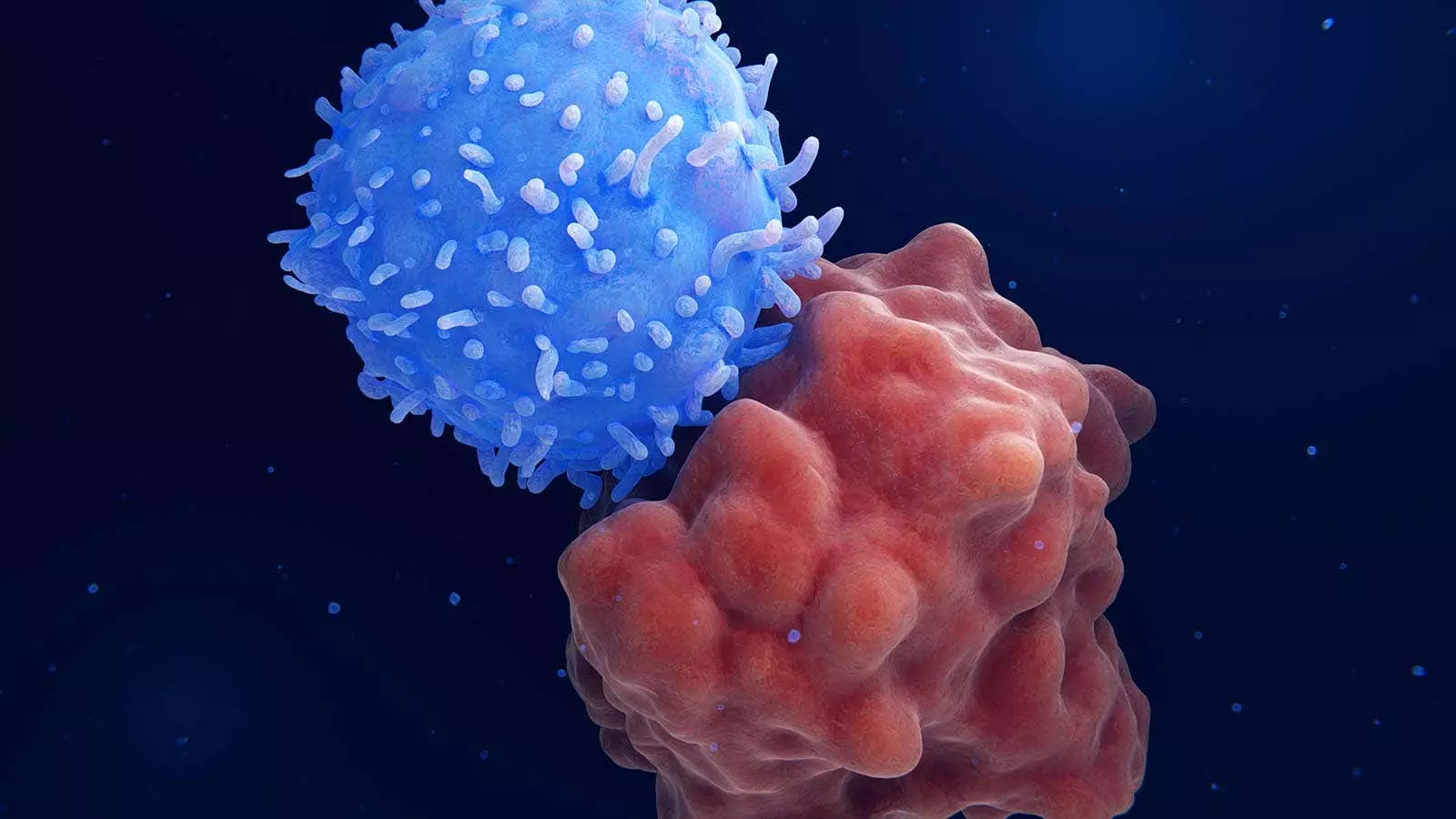
A recent study conducted by Chinese researchers introduced an innovative strategy involving sequential CD7 chimeric antigen receptor (CAR) T-cell therapy followed by haploidentical hematopoietic stem-cell transplantation (HSCT) for patients with relapsed or refractory hematologic cancers. This groundbreaking approach, which eliminates the need for graft-versus-host disease (GVHD) prophylaxis, has shown promising results in terms of complete remission and overall survival rates.
After receiving CAR T-cell therapy, all 10 patients in the study achieved complete remission, with nine of them exhibiting minimal residual disease (MRD)-negative incomplete hematologic recovery. Subsequently, nine patients underwent haploidentical HSCT within 1 month of the initial therapy. The results, with a median follow-up of 15.1 months, revealed a 1-year overall survival rate of 68% and a 1-year disease-free survival rate of 54%. This novel approach creates a specific condition for successful allogeneic HSPC engraftment, GVHD control, and concomitant CAR T-cell persistence, offering a new strategic option for allogeneic HSCT.
The study’s findings, though preliminary, have opened up areas of exploration for further research and application. The strategy is being considered as a first-line treatment for patients with CD7-positive acute myeloid leukemia (AML) who cannot undergo intensive induction therapy. Additionally, the possibility of incorporating dual CAR T-cell constructs targeting both CD7 and another antigen for CD7-negative leukemia is being explored. This all-in-one approach holds promise for advancing treatment paradigms, particularly in challenging cases of AML with a poor prognosis.
The patients enrolled in the study presented with relapsed or refractory CD7-positive leukemia or lymphoma. The median age at enrollment was 56.5 years, with 60% of participants being women. These individuals had undergone extensive prior treatment, with a median of 9.5 previous courses of therapy. The majority had AML, while others had T-cell acute lymphoblastic leukemia or T-cell lymphoblastic lymphoma. The overall response to the treatment strategy was positive, with a notable decrease in MRD and favorable remission rates.
While the treatment approach demonstrated efficacy in inducing remission and improving survival rates, several patients experienced complications and adverse events. Cytokine release syndrome (CRS) was observed in nine patients, with all cases being grade 1 or 2 and successfully controlled. Additionally, four patients developed grade 2 GVHD, but no cases of chronic GVHD were reported. Several patients suffered from severe infections, ultimately leading to fatalities in two cases. The management of infections and complications remains a critical aspect of the treatment strategy.
The innovative strategy of sequential CD7 CAR T-cell therapy followed by haploidentical HSCT represents a promising approach for patients with relapsed or refractory hematologic cancers. The results of the study suggest significant benefits in terms of complete remission rates, disease-free survival, and overall outcomes. Further research and clinical trials are needed to validate these findings and optimize the treatment protocol for broader applicability in clinical practice.


Leave a Reply