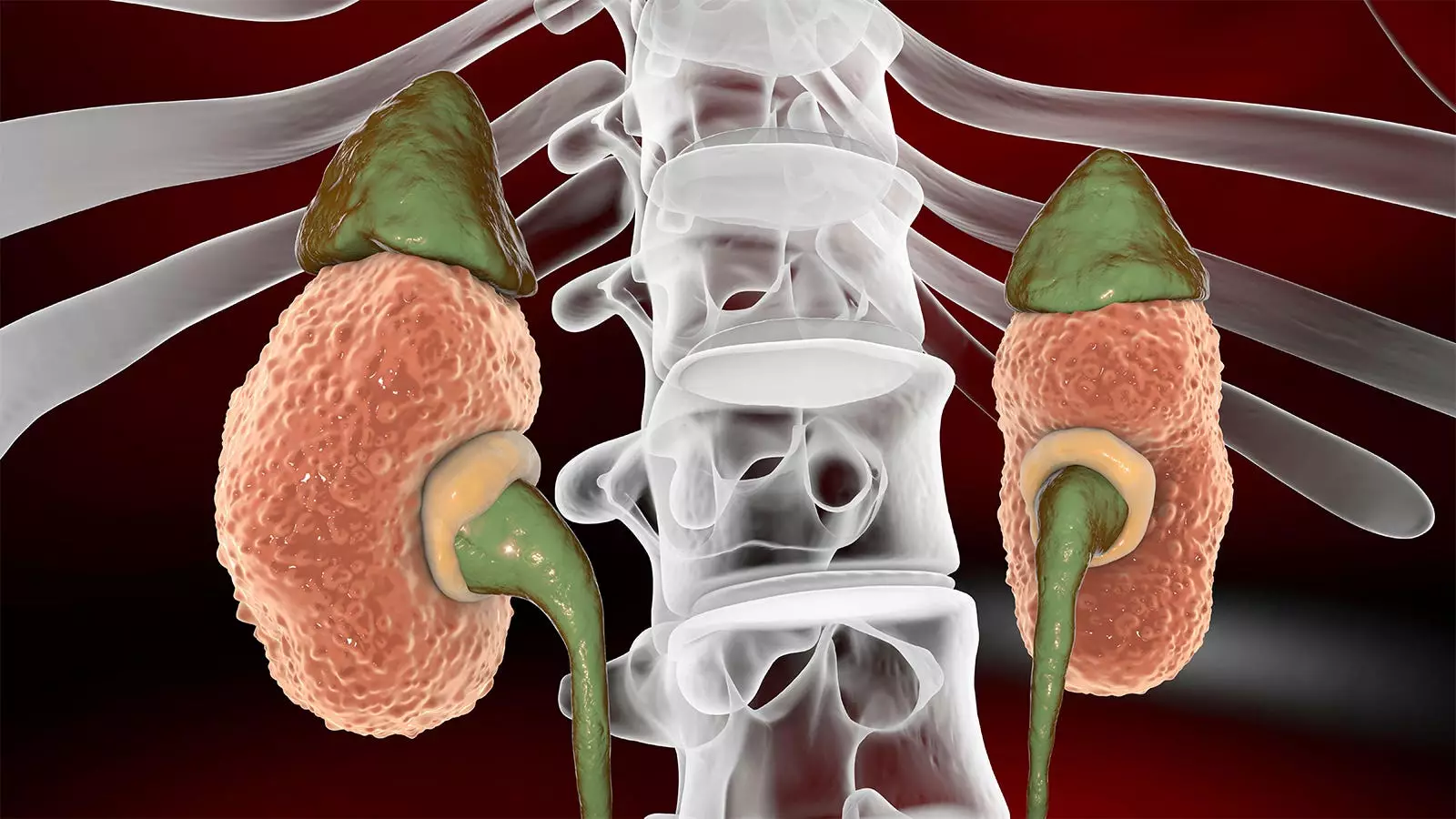
As a Black physician, I have witnessed firsthand the cultural tendencies in communities of color to avoid discussing or disclosing health issues, even to family members. This trend is particularly noticeable in patients diagnosed with autosomal dominant polycystic kidney disease (ADPKD). ADPKD is a rare genetic disorder that affects over 140,000 adults in the U.S., leading to the formation of fluid-filled cysts in the kidneys that can result in the replacement of normal kidney tissue and a decline in kidney function. However, due to cultural norms, many patients of color delay seeking medical help until the disease progresses to a later stage, hindering the effectiveness of management strategies that could have been implemented earlier.
Patients of color may face misdiagnosis or delayed diagnosis of ADPKD due to various risk factors that disproportionately affect them. Conditions such as hypertension and diabetes, which are prevalent in Black and Hispanic populations, can mask the symptoms of ADPKD and lead to delayed screenings. In some cases, hypertension, which occurs in a significant number of ADPKD cases, may be mistaken for an environmental or lifestyle-related issue, further complicating the diagnostic process. This delay in diagnosis can be detrimental, as early intervention is crucial to managing the disease effectively.
Diagnosing ADPKD can be challenging, especially in patients of color, as the disease may present with normal or slightly reduced kidney function despite significant progression. Black patients, in particular, may experience a more rapid decline in kidney function, making it essential to focus on kidney size rather than kidney function when assessing disease progression. Factors such as family history, weight, and protein levels in the urine can also impact the rate of disease progression and should be taken into consideration during diagnosis.
In addition to physical factors, patients of color may face structural and cultural barriers that impede their access to medical care and timely diagnosis. Uninsured individuals or those living in communities with limited healthcare resources are at a higher risk of being diagnosed with renal failure when the disease has already reached an advanced stage. Overcoming these obstacles requires a concerted effort to improve access to healthcare services and raise awareness about the importance of early intervention in managing ADPKD.
Encouraging open conversations about ADPKD within families and providing education about the disease are crucial steps in addressing the challenges faced by patients of color. Genetic screening and early detection can help identify at-risk individuals and enable them to make informed decisions about their health. Supporting patients through their journey with ADPKD and connecting them with resources and support groups can also improve health outcomes and quality of life.
Addressing cultural tendencies, risk factors, and structural barriers in diagnosing ADPKD in communities of color is essential to improving healthcare outcomes and reducing disparities in treatment. By prioritizing early detection, education, and support for patients, healthcare providers can enhance the quality of care and support patients in managing their condition effectively. Collaboration among healthcare professionals, patients, and community organizations is key to overcoming the challenges faced by patients of color with ADPKD and ensuring equitable access to care.


Leave a Reply