Chronic inflammatory demyelinating polyneuropathy (CIDP) is a complex disease that often goes undiagnosed or misdiagnosed due to its rarity and heterogeneity. Current standard treatments like intravenous immunoglobulin (IVIG), steroids, and plasma exchange have limitations in some CIDP phenotypes, making the need for valid biomarkers crucial.
Dr. Jeffrey Allen of the University of Minnesota highlights the urgency for biomarkers in CIDP to improve diagnosis accuracy and treatment understanding. Over the years, researchers have explored various potential biomarkers such as autoantibodies, cytokines, complement proteins, and IgG levels. Despite this extensive search, CIDP still lacks widely accepted biomarkers due to the diverse mechanisms at play in the disease.
Potential Fluid Biomarkers
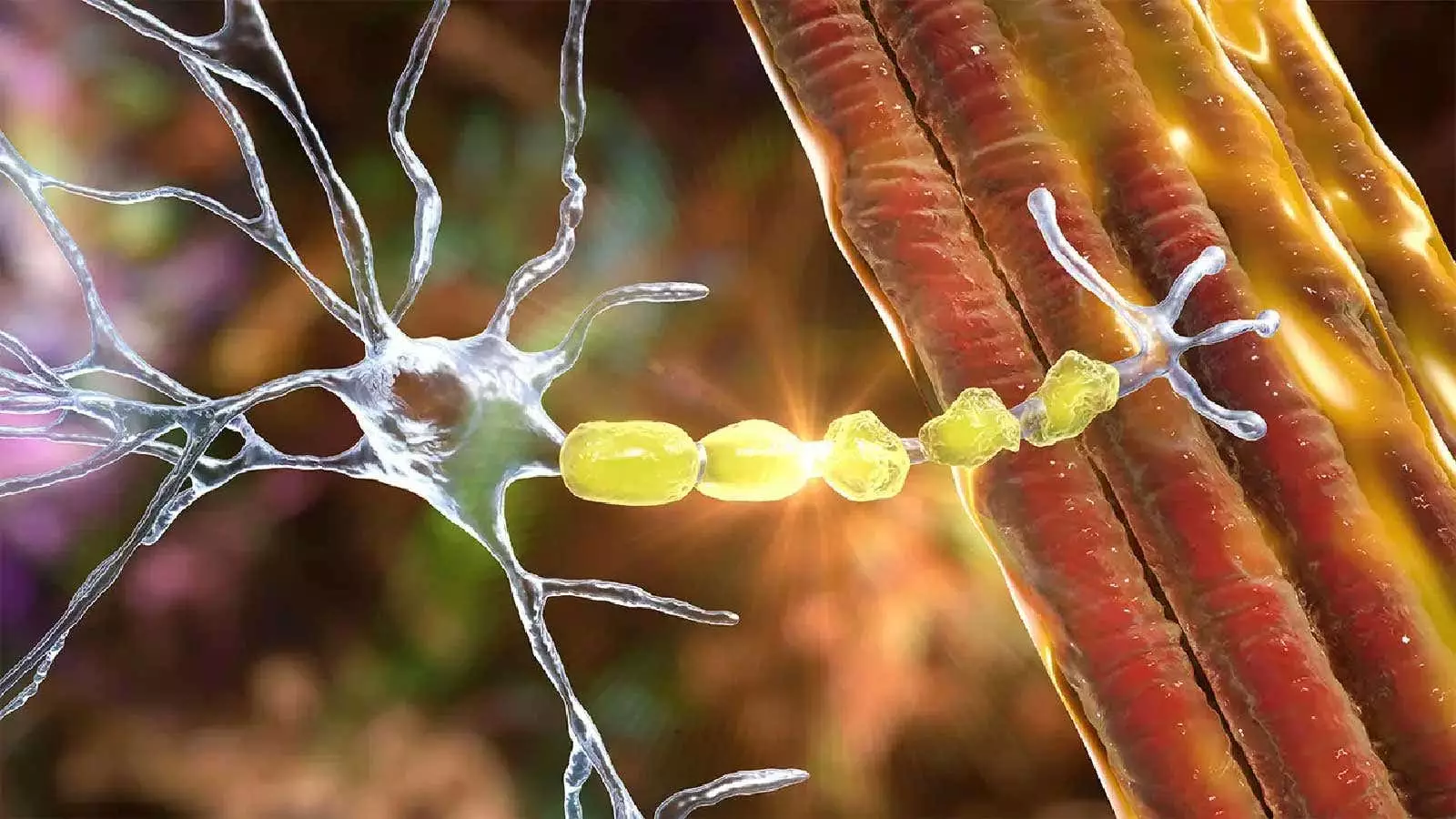
One promising fluid biomarker for CIDP is the serum neurofilament light chain (NfL), reflecting axonal damage and predicting poor outcomes in CIDP patients. Studies have shown elevated levels of serum NfL in some CIDP patients, indicating its potential as a disease activity biomarker. Additionally, antibodies such as anti-neurofascin-155 and anti-contactin-1 have emerged as potential biomarkers for autoimmune nodopathies in CIDP, aiding in therapeutic decisions.
Cerebrospinal fluid (CSF) has also been a target for biomarker exploration in CIDP, with studies focusing on interleukin-8 (IL-8) levels and autoantigen repertoire. These efforts aim to differentiate CIDP from other neurological disorders and improve treatment responsiveness. Ongoing projects like the INCbase study are dedicated to collecting bio-samples from a diverse group of CIDP patients to identify diagnostic and disease activity biomarkers.
Imaging Techniques in CIDP
Imaging plays a crucial role in assessing damage in CIDP and complementing traditional diagnostic methods like nerve conduction studies and electromyography. Whole-body magnetic resonance neurography (MRN) has shown promise in providing clear images of nerve continuity, integrity, and pathological changes in CIDP patients. Researchers have identified significant imaging findings in CIDP patients using MRN, highlighting its potential in enhancing diagnostic accuracy and treatment monitoring.
Ultrasound imaging has also gained attention in CIDP diagnosis, particularly in distinguishing immune neuropathies from controls. High-frequency ultrasound of nerve structures can aid in diagnosing CIDP when combined with clinical criteria, such as nerve enlargement in specific segments. The EAN/PNS guideline recommends using ultrasound and MRI to enhance CIDP diagnosis in adults meeting diagnostic criteria, emphasizing the importance of detailed imaging in comprehensive evaluation.
The quest for biomarkers and advanced imaging techniques in CIDP continues to evolve, aiming to enhance diagnostic accuracy, treatment decisions, and disease monitoring. As researchers delve deeper into the complexities of CIDP, identifying reliable biomarkers and implementing innovative imaging modalities will be crucial in improving patient outcomes and advancing the understanding of this challenging neurological disorder.


Leave a Reply