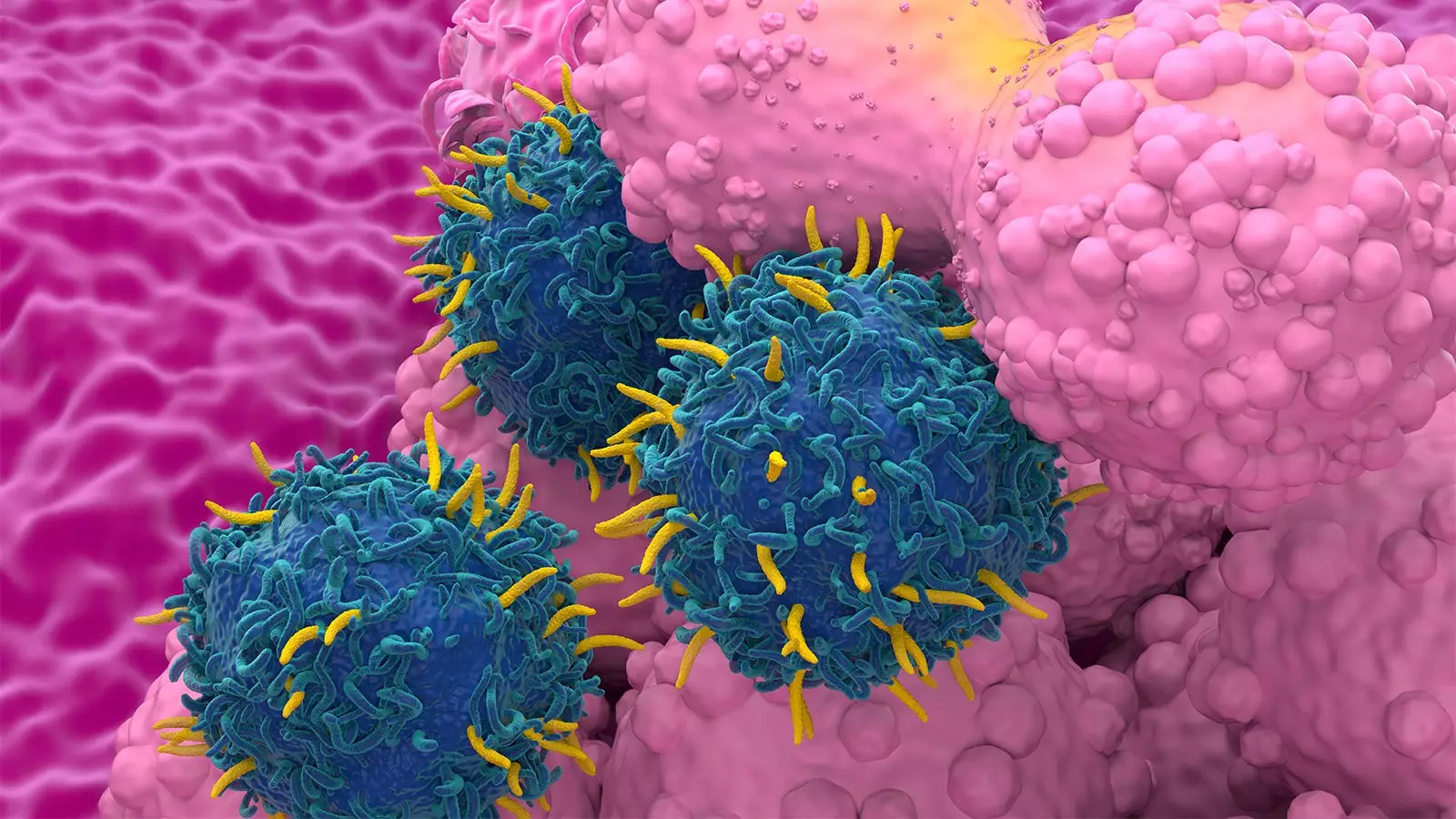
CAR T-cell therapy has become a promising treatment option for patients with cancer, showing potential for long-term remission and even cure. However, recent reports have raised concerns about the risk of second primary malignancies (SPM) associated with this therapy. A systematic literature review and meta-analysis aimed to shed light on this issue and compare the risk of SPM with CAR T-cell therapy to that of other standard-of-care (SOC) cancer therapies.
The analysis revealed a 5.8% rate of SPM among 5,517 patients with a median follow-up of 21.7 months. Interestingly, the rate of SPM did not vary according to the type of disease treated or the specific CAR T-cell product used. Factors such as study setting, longer duration of follow-up, and the number of therapies prior to CAR-T treatment were associated with a higher rate of SPM. Despite concerns raised by the FDA and previous reports, the meta-analysis showed virtually identical rates of SPM between CAR T-cell therapy and SOC treatments.
While the findings suggest that the risk of SPM with CAR T-cell therapy may not be as significant as initially feared, there are still concerns about potential biases in the adverse-event (AE) data used for the analysis. Proper assessment of SPM risk should account for various confounders such as patient age, follow-up duration, and previous treatments received. The need for more long-term data to better understand the factors underlying SPM was highlighted in the study.
Patients receiving CAR T-cell therapy may understandably have questions and concerns about the potential risks associated with this treatment. It is crucial for providers to interpret the data cautiously and provide appropriate context to their patients. The study emphasizes the importance of thorough monitoring and follow-up, especially for patients with longer follow-up duration and multiple lines of prior therapy.
The analysis identified a total of 326 SPMs, with hematologic malignancies being the most common type observed. Interestingly, T-cell malignancies, which are of particular interest with CAR T-cell therapies, accounted for a small percentage of the SPMs. The association between follow-up duration and SPM rate underscores the need for continued surveillance and monitoring of patients receiving CAR T-cell therapy. More research is needed to better understand the underlying factors contributing to SPM and to improve the long-term outcomes for patients.
While there are concerns about the risk of SPM with CAR T-cell therapy, the analysis suggests that the risk may not be significantly higher compared to other SOC cancer therapies. Providers should remain vigilant and continue to monitor patients closely, especially those with longer follow-up durations and multiple prior lines of therapy. Further research is needed to address the gaps in understanding and to improve the safety and efficacy of CAR T-cell therapy for patients with cancer.


Leave a Reply