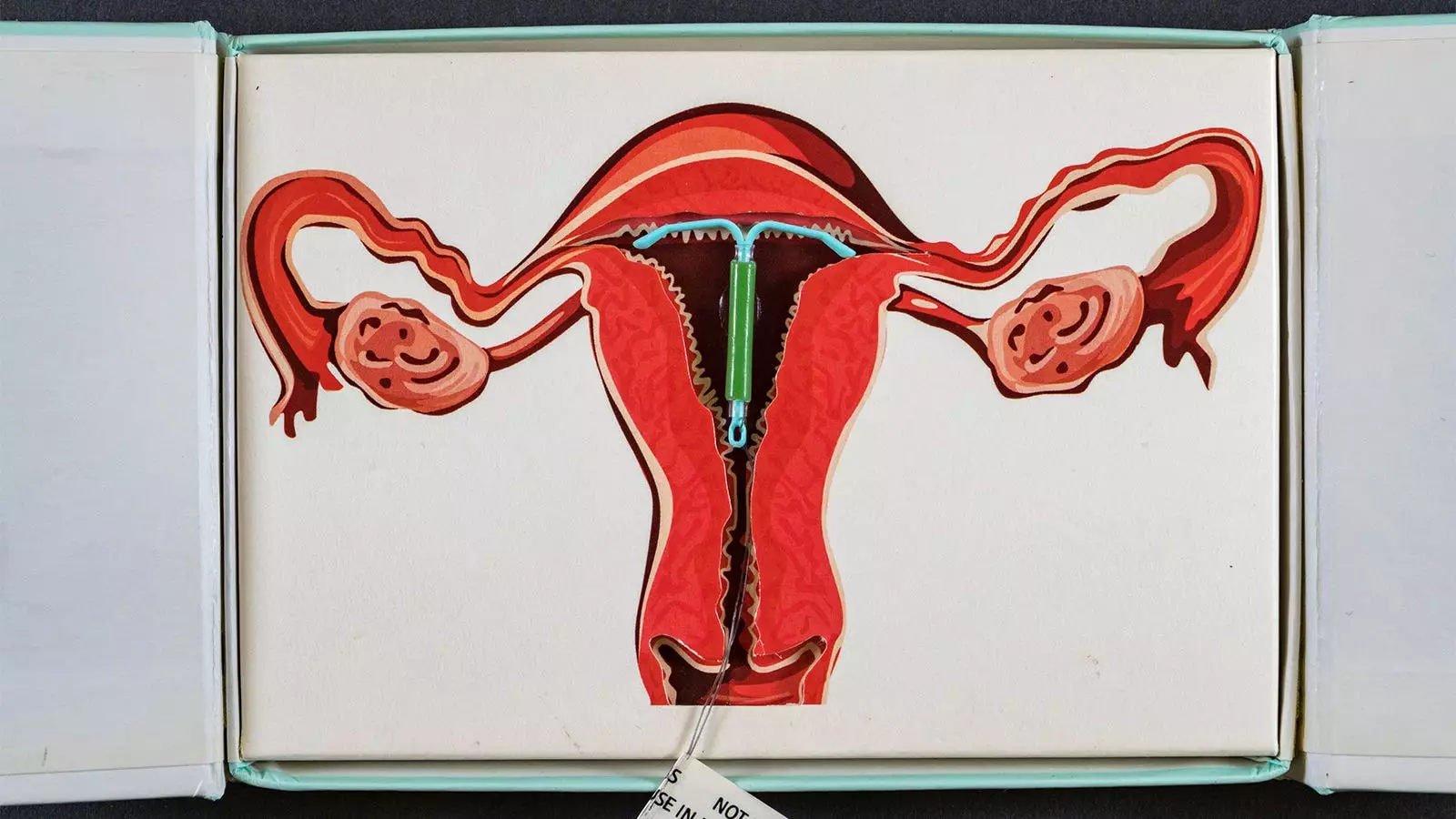
The use of hormonal contraceptives, particularly levonorgestrel-releasing intrauterine devices (IUDs), has become increasingly prevalent among women of reproductive age. However, emerging research raises vital questions about the potential long-term health risks associated with these contraceptive methods. A recent Danish study has highlighted a substantial link between the use of hormone-releasing IUDs and an elevated risk of breast cancer in women under 50. This article critically evaluates the findings of the study, exploring its implications for women’s health and reproductive choices.
Conducted by Lina Steinrud Mørch and colleagues from the Danish Cancer Institute, the investigation focused on almost 79,000 first-time users of levonorgestrel-releasing IUDs from 2000 to 2019. Notably, the study also considered a control group of non-users, matched in demographic and health characteristics. Over the follow-up period of roughly seven years, the researchers found that users of these contraceptives had an approximate 40% increased risk of breast cancer compared to non-users, with risk further amplifying with prolonged use.
The categories of hormone-releasing IUD use demonstrated distinct hazard ratios relating to breast cancer diagnoses. For durations of use spanning 0-5 years, the hazard ratio stood at 1.3; for 5-10 years at 1.4; and for more than a decade, it reached as high as 1.8. These ratios translate into alarming rates of excess breast cancer diagnoses, particularly for those utilizing the devices over longer periods, with implications that could affect thousands of women. However, the study’s authors have also warned that the observed trends may not be statistically significant, indicating that further investigation is warranted before drawing definitive conclusions.
The findings prompt essential conversations regarding the safety and health ramifications of choosing hormonal contraceptives, especially for young women who may have long-term plans for their contraception strategy. With breast cancer being one of the most common cancers affecting women globally, the potential heightened risk attached to a popular contraceptive method necessitates careful consideration. The study calls for a more robust communication framework between healthcare providers and patients, where the long-term risks associated with IUDs are clearly articulated alongside their benefits.
Previous studies have documented mixed findings on the association between hormonal contraceptives and cancer risk. Some earlier research indicated that the hazard ratios for breast cancer among users of hormonal contraceptives were comparable to those for short-term levonorgestrel IUD usage. Yet, a crucial limitation in past studies lies in their inability to sufficiently address the influence of varying durations of contraception use and different types of hormonal methods. The current research adds valuable data to the ongoing discourse, particularly in recognizing the potentially cumulative risk that prolonged exposure to hormonal contraceptives may impart.
Despite its robust sample size and detailed methodology, the Danish study is not without its limitations. The possibility that women may have discontinued IUD use before the recommended duration could result in an underestimation of breast cancer risk. Additionally, unmeasured confounding variables—such as lifestyle factors, genetic predispositions, or environmental influences—could skew the results. The authors themselves acknowledge these limitations, suggesting that the absence of a consistent dose-response relationship may indicate either a lack of statistical power in their analysis or a non-causal association altogether.
The link between levonorgestrel-releasing IUDs and increased breast cancer risk raises critical questions for women’s health and contraceptive use. This study emphasizes the importance of informed decision-making, advocating for transparency between healthcare professionals and patients concerning the potential risks and benefits associated with hormonal contraceptives. Ultimately, future research must not only seek to clarify the complex relationship between hormonal contraception and various health risks but also strive to enhance women’s understanding of their reproductive choices, enabling them to make well-informed decisions that safeguard their long-term health.


Leave a Reply