The recent approval of Eli Lilly’s anti-obesity drug, Zepbound, for patients with obstructive sleep apnea (OSA) has generated significant discussion regarding its implications for Medicare drug plans. With OSA affecting a large population in the United States, this development could drastically change access to treatment options for individuals suffering from both obesity and sleep-related breathing disorders. Understanding the coverage intricacies alongside the drug’s potential benefits and economic considerations is essential in evaluating this health care policy shift.
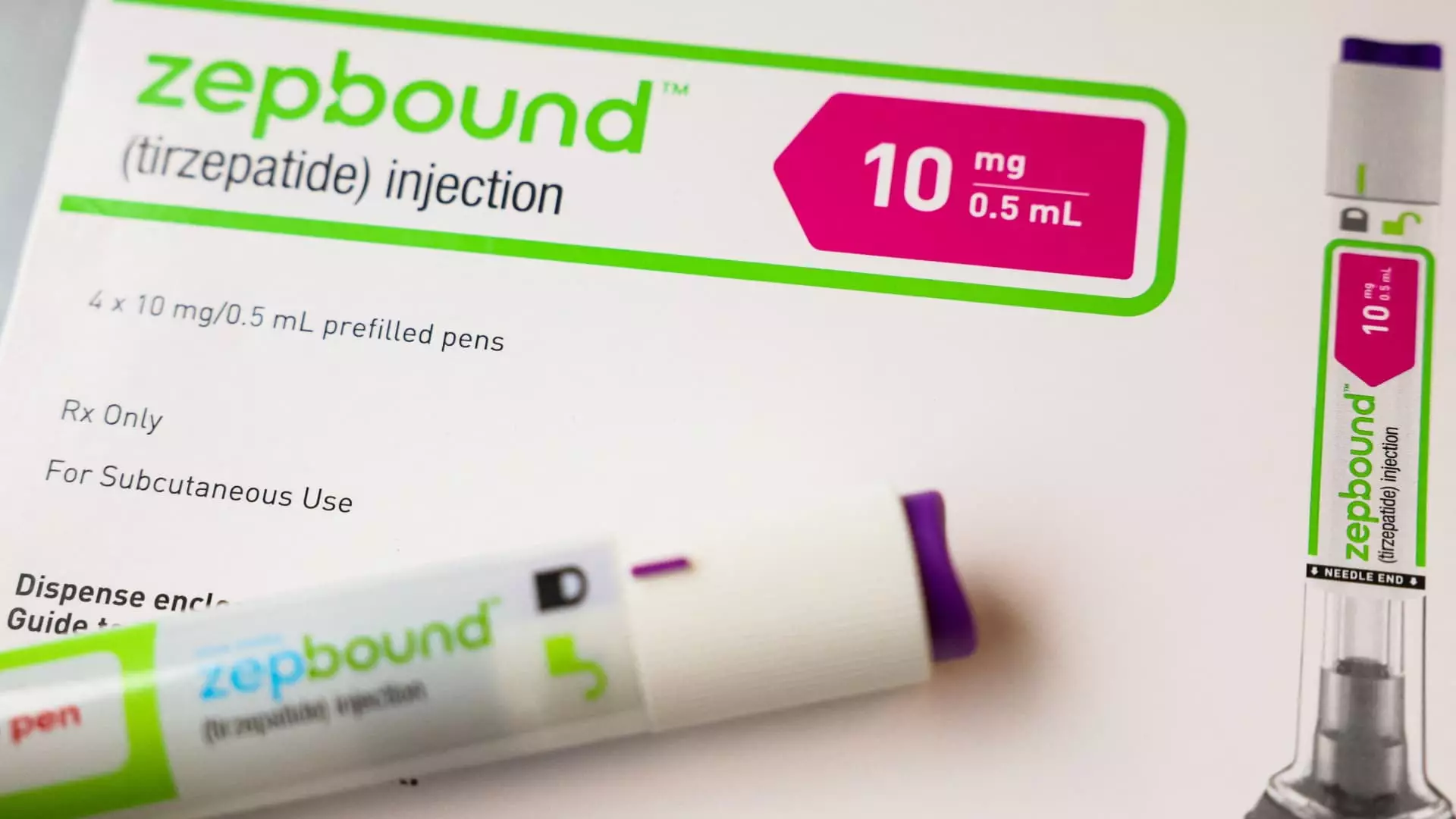
Eli Lilly’s Zepbound received federal approval on December 20 for use in individuals battling moderate-to-severe forms of OSA, adding a crucial tool to the arsenal for managing a common yet often overlooked condition. According to estimates, around 20 million individuals suffer from OSA, which can lead to additional health issues like cardiovascular disease and increased risk of diabetes. By designating Zepbound as an approved treatment for this condition, the FDA acknowledges its potential to not only address obesity but also improve health outcomes for patients with specific medical needs.
The economic burden associated with these health issues heightens the necessity for affordable treatment options. With Zepbound’s initial price around $1,000 before insurance, its cost can deter access for many patients. The integration of Zepbound into Medicare drug plans signifies an important step toward making effective medication more accessible. However, a notable limitation remains in the existing legislation concerning coverage criteria and the approval processes that all drugs must navigate.
Despite the potential for broader access, the coverage rules surrounding Zepbound raise important questions about the efficacy of present healthcare policies. Under Medicare Part D guidelines, medications designed for obesity treatment require a justification of necessity based on medically accepted purposes per FDA approval. As per communications from the Centers for Medicare & Medicaid Services (CMS), these plans may invoke prior authorization to ensure drugs, like Zepbound, are prescribed for indicated conditions, like OSA.
This creates a convoluted landscape for physicians and patients. Instead of simple access to necessary medications, healthcare providers face additional bureaucracy that could delay treatment. The variability in state Medicaid programs further complicates this scenario, as coverage can depend heavily on manufacturer agreements and the specific health conditions for which drugs are prescribed. Therefore, while Zepbound’s entry into Medicare drug coverage marks progress, many hurdles still prevent its full potential from being realized in practice.
In conjunction with ongoing studies into the effectiveness of Zepbound and similar medications for various conditions, including fatty liver disease and chronic kidney disease, the implications extend beyond just obesity or sleep apnea. If Eli Lilly and Novo Nordisk successfully establish further uses for their medications, the landscape of drug coverage in Medicare and Medicaid could shift dramatically.
An important concern surrounding this expansion of drug coverage stems from budgetary constraints on government spending. The Biden administration proposed a policy allowing Medicare and Medicaid to cover weight loss medications for patients classified as obese, but this could impose an additional $35 billion burden over ten years. The debate lies in balancing the growing need for accessible medical treatments against the potential strain on public resources.
The approval of Zepbound for obstructive sleep apnea is undoubtedly a significant advancement in the realm of obesity treatments, particularly concerning Medicare coverage. While the potential for enhanced access to effective medications is promising, complexities in policy and economic ramifications remain critical to understand. As the landscape of healthcare and pharmaceutical efficacy evolves, continued dialogue among legislators, medical professionals, and patients will be essential to ensure that healthcare policies adapt in a way that balances fiscal responsibility with the imperative of comprehensive patient care. As we look to the future, it will be crucial for policymakers to consider both the clinical benefits and the associated costs of new therapies in devising strategies for sustainable healthcare financing.


Leave a Reply