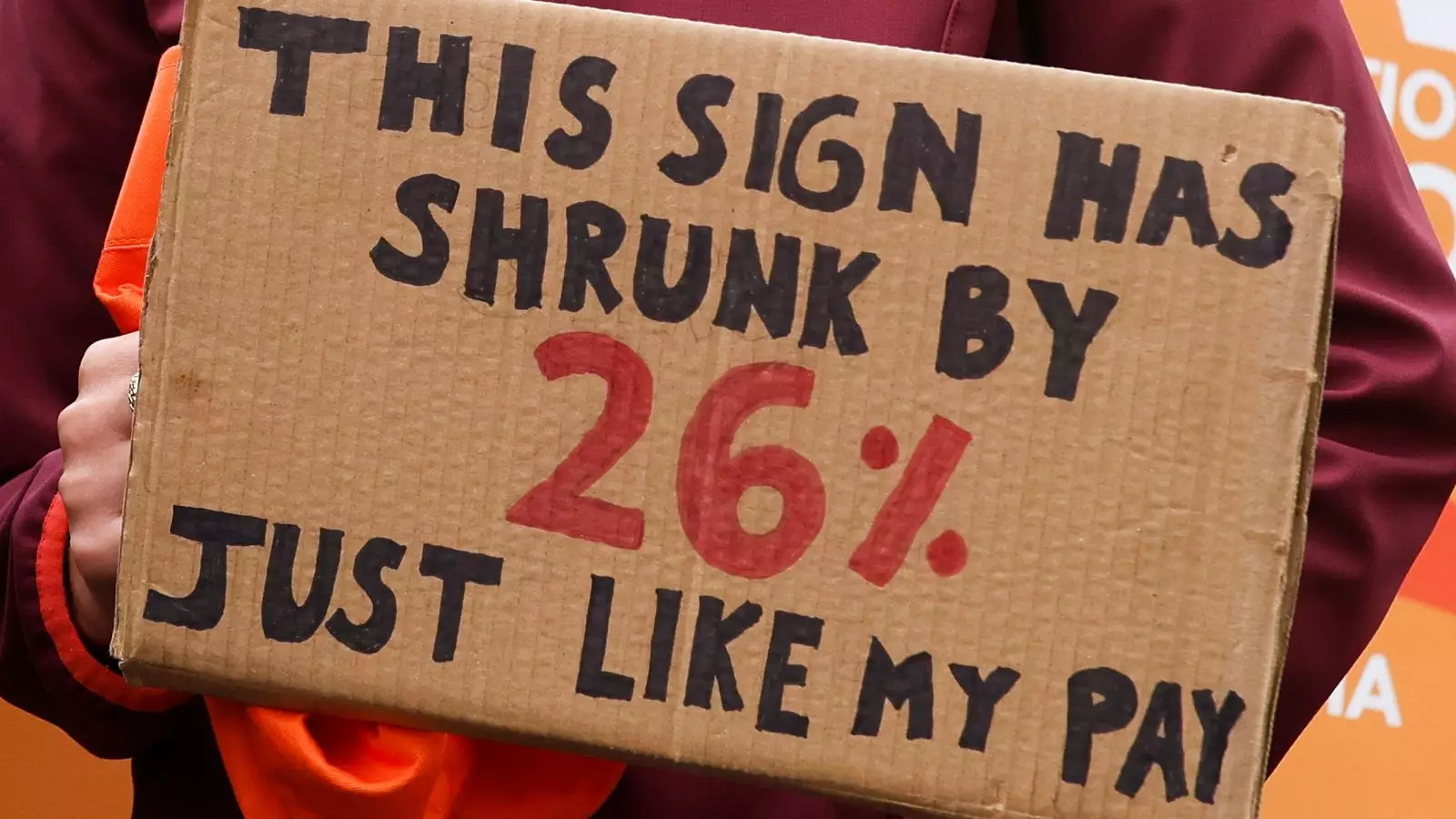
The ongoing dispute between resident doctors and the NHS management exposes a deeper failure in how the health system values its frontline workers. At the heart of this conflict is a simple yet profound question: How much should healthcare professionals be compensated for their vital work? The BMA’s demand for a 26% pay restoration highlights longstanding grievances about stagnating wages and underpayment, which have persisted for nearly two decades. From an ethical standpoint, this is not merely a financial matter but a moral one—how a society cares for the caregivers who sustain its health. The current salary—roughly £18 per hour—does little to reflect the immense responsibility resting on these young professionals, many of whom work demanding shifts with little room for personal stability.
Yet, the response from the government, particularly Secretary of State Wes Streeting, has been characterized by resistance rather than recognition of these systemic issues. While public discourse depicts the dispute as a straightforward financial clash, it masks the reality that the NHS’s reforms hinge precariously on the goodwill and morale of its staff. Cutting corners—refusing to acknowledge that underpayment fuels burnout and attrition—threatens to undermine the very fabric of NHS functionality. The argument that staff have already received significant pay rises does little to address the decades of underfunding and undervaluation that have left a generation of doctors feeling betrayed.
The Illusion of Local Autonomy and Its Hidden Risks
In an effort to defuse the crisis, the government has proposed granting local NHS trust leaders more authority to manage service delivery during strikes. While decentralizing decisions appears pragmatic, it risks escalating a fragile situation into chaos. Trust leaders, though better acquainted with their immediate teams, are fundamentally limited by structural constraints. They lack the robust authority and resources needed to ensure patient safety in the face of widespread staff shortages caused by strikes and backfill personnel.
This approach effectively shifts blame onto local managers, suggesting that hospitals can simply “prioritize urgent cases” without acknowledging the systemic failure of workforce planning. The danger lies in a piecemeal approach that treats the symptoms but ignores the root cause—an undervalued workforce under pressure for nearly two decades. Relying on locally negotiated decisions creates inconsistency, leaving patients uncertain and vulnerable. For conditions like cancer treatment or emergency care, where timing is critical, this patchwork solution risks exacerbating health inequalities and eroding public trust.
The Politics of Neglect and the True Cost of Underinvestment
Both sides, in this high-stakes confrontation, rarely address the fundamental issue: chronic underfunding that has gnawed at the NHS’s core for years. The government’s narrative of “already providing significant pay increases” is misleading when juxtaposed with the reality of a service stretched to its breaking point. The NHS’s financial and staffing crises are not incidental; they are the logical consequence of a system that prioritizes austerity over investment, efficiency over the well-being of its staff.
The escalation of this dispute is a symptom of a broader political failure—a refusal to prioritize health care as a societal right. Instead, successive governments have allowed the NHS to operate under the guise of efficiency, often sacrificing quality and staff morale in pursuit of short-term budgetary gains. This moment should serve as a wake-up call: the health service’s sustainability depends on genuine investment and a recognition that the backbone of healthcare delivery are those who provide it. Ignoring their needs under the guise of fiscal discipline ultimately endangers everyone and betrays the foundational promise of universal healthcare.


Leave a Reply