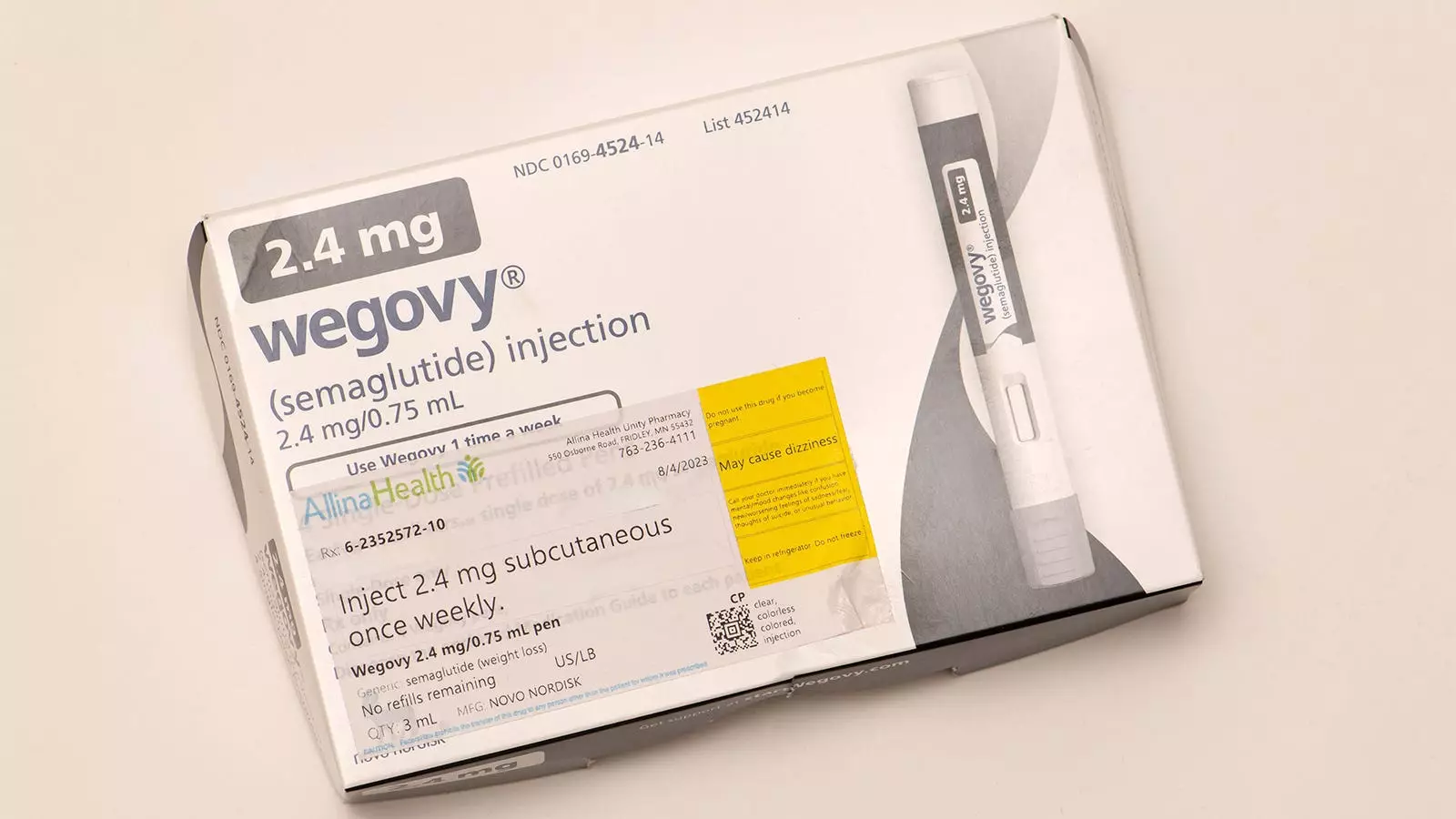
The rising prevalence of obesity in children and adolescents is an urgent public health crisis, prompting the need for effective treatment strategies. As a pediatric obesity medicine specialist, I have had firsthand experience with the limitations of current treatment modalities and have keenly observed the potential of GLP-1 receptor agonists, particularly semaglutide (marketed as Wegovy), in managing obesity in older adolescents. My professional practice is particularly focused on applying these treatments in combination with intensive lifestyle interventions, yielding improvements in both metabolic and psychosocial dimensions for the older demographic.
The Current Landscape of Childhood Obesity Treatment
Despite the advancements in medication for adolescents, the situation is starkly different for younger children under the age of 12. Strikingly, these younger patients present a paradox; despite the severity of their obesity and associated comorbidities—such as prediabetes, fatty liver disease, and sleep apnea—there are no approved pharmacological treatment options available. This gap in treatment options becomes even more pronounced when considering the potential psychological impacts, such as bullying and social stigma, that many of these children face.
However, a ray of hope is on the horizon. The FDA is currently reviewing liraglutide, another GLP-1 receptor agonist that could set a precedent for pharmacological intervention in younger populations. Recently published research in the New England Journal of Medicine indicates that liraglutide, when combined with a comprehensive lifestyle intervention, may be effective for children ages 6 to 12 suffering from severe obesity.
Study Insights: A Closer Look
The randomized clinical trial involved 82 children over a 56-week period, highlighting significant outcomes. Children who received liraglutide reported a decrease in body mass index (BMI) of 5.8%, whereas those only undergoing lifestyle interventions saw a BMI increase of 1.6%. While these figures are eye-catching, it is crucial to assess such data critically. Nearly 80% of those receiving liraglutide experienced gastrointestinal side effects, although most were classified as mild to moderate. This raises the essential question of whether the benefits of treatment truly justify these potential side effects, especially given that the majority of these side effects can impact a child’s quality of life.
Furthermore, the trial did not yield statistically significant improvements in metabolic markers such as blood pressure or hemoglobin A1c. Such findings highlight a crucial point: although modest benefits may exist, especially around BMI reduction, the improvements in metabolic health are not as pronounced as one would hope, leaving both patients and clinicians with more questions than answers.
The promise of pharmacological treatments such as liraglutide hinges heavily on a thorough understanding of their long-term safety and efficacy. Based on the trial results, while the short-term BMI reductions are appealing, concerns linger regarding their long-term implications on factors like growth and ultimate adult height, potential unknown side effects, and the likelihood of weight regain once medication cessation occurs. In this regard, the alarming statistic of children in the treatment group regaining nearly all lost weight upon stopping the medication must not be taken lightly.
Moreover, the requirement of daily injections introduces another layer of complexity and potential compliance issues, particularly in younger children who may be reluctant to engage in such a routine.
The treatment of severe obesity is undoubtedly multifaceted and must be approached with a tailored strategy. GLP-1 medications may eventually serve a meaningful role for some children aged 6-12—an age group that greatly needs these options—yet the conversation must be grounded in a careful analysis of risks and benefits.
As clinicians, we carry the responsibility of discussing these factors with caregivers and ensuring that any chosen intervention includes comprehensive lifestyle modifications. My position, as it currently stands, leans toward prioritizing non-pharmacological interventions over medications, as long-term data are still needed to elucidate the implications of using these drugs in a younger population.
The Path Forward for Pediatric Obesity Management
While the potential FDA approval of liraglutide represents a significant step forward in pediatric obesity management, it is vital that we proceed with caution. The research community plays a pivotal role in advancing our understanding of obesity treatments in children, and I am hopeful that further studies will provide the robust data necessary to inform our clinical decisions in the future.
While the emergence of GLP-1 receptor agonists like liraglutide may change the landscape of childhood obesity treatment, it is essential that professionals remain critical and cautious as we navigate the intricate balance between benefits, risks, and the unique needs of our younger patients.


Leave a Reply