Aging is a complex biological process that not only affects physical health but also influences the risk of developing various diseases, including cancer. Researchers have long observed a J-shaped curve in cancer risk associated with age, emphasizing an increase in susceptibility during midlife, followed by a decline in risk in the later decades. This article investigates the recent insights into this paradox and the cellular mechanisms involved, focusing on a new study examining lung cancer development in older mice.
Cancer risk is generally perceived to escalate as individuals enter their 60s and 70s due to the accumulated effects of genetic mutations and environmental exposures over time. During this period, the body’s repair mechanisms may also weaken, further compounding the risk. However, a puzzling phenomenon occurs around the age of 80, where the incidence of certain cancers appears to diminish. The understanding of this decline has been largely speculative, but recent research provides a clearer picture of the underlying biochemical processes.
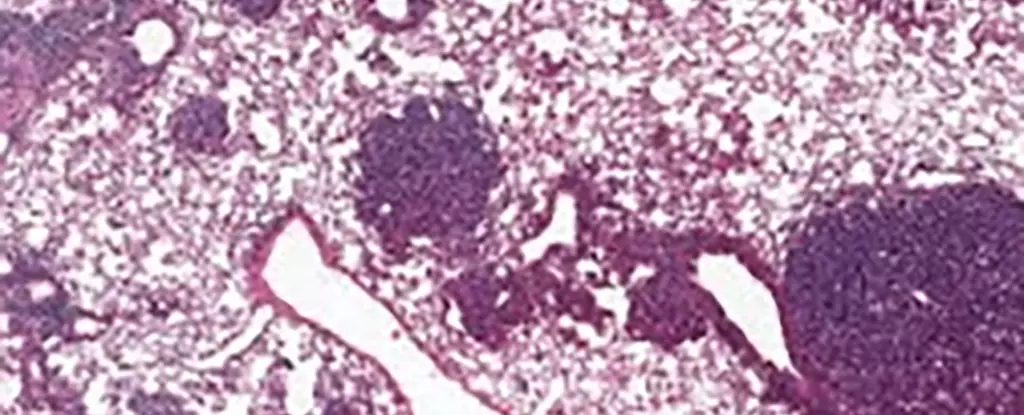
The latest study, conducted by an international team including cancer biologists from prestigious institutions, examined the role of specific stem cells in lung cancer development. In particular, the focus was on alveolar type 2 (AT2) stem cells, which are pivotal for lung regeneration and are often where lung cancers originate. By analyzing these cells in older mice, the researchers unveiled significant findings related to the protein NUPR1.
The study identified elevated levels of NUPR1 in aging mice, which seemed to promote a functional iron deficiency in AT2 cells. This paradoxical effect means that despite an abundance of iron in aging cells, their functionality resembled that of cells that lacked iron. Researcher Xueqian Zhuang stated that these aging cells lose the capacity to regenerate, thereby limiting both healthy growth and the proliferation of cancerous tumors. This phenomenon could explain why older individuals may experience a reduced risk of cancer despite their decades of genetic damage.
Moreover, when researchers manipulated NUPR1 levels or increased iron availability in the cells, they observed a revival in cell growth capabilities. This suggests a potential therapeutic avenue that revolves around iron metabolism, particularly for older individuals who could be facing various lung health challenges, including post-COVID-19 symptoms.
The findings have far-reaching implications for cancer treatment strategies, especially those that leverage a process known as ferroptosis—a form of cell death initiated by iron accumulation. The study suggests that older cells exhibit a resistance to ferroptosis, which could hinder the efficacy of emerging treatments targeting this pathway. This presents a crucial insight: initiating ferroptosis-based therapies earlier in patients’ lives may enhance treatment outcomes.
Moreover, the research underscores the importance of preventative measures against known carcinogens. Tuomas Tammela, another researcher involved, pointed out that the risks posed by certain lifestyle choices in youth, such as smoking and excessive sun exposure, are perhaps more critical than previously recognized. Addressing these modifiable factors in younger populations remains a key aspect of cancer prevention.
As the study illustrates, the relationship between aging and cancer risk is intricate, warranting further exploration. While this research has highlighted NUPR1 as a critical factor influencing the behavior of stem cells, there remains much to uncover about the biological transformations that occur with aging and their implications for cancer pathophysiology.
Personalization in cancer treatment, taking into account the individual’s age, overall health, and the specific characteristics of their cancer, is becoming increasingly crucial. As Zhuang noted, understanding how aging alters cancer biology opens new avenues for targeted and more effective interventions across different life stages.
The insights gained from this study not only pave the way for potential therapeutic strategies but also call on the medical community to continue investigating the complex interplay of aging, cellular behavior, and cancer development. Only through such detailed inquiry can we hope to improve outcomes and quality of life for all patients navigating the challenges of cancer in an aging population.


Leave a Reply